What Is Vasa Previa?
Vasa previa occurs when a fetal blood vessel or vessels from the placenta or umbilical cord cross the entrance to the birth canal in front of the baby. Vasa previa can result in rapid fetal hemorrhage if the vessels tear when the cervix dilates or the membranes of the amniotic sac rupture.
The aberrant vessels may be caused by velamentous insertion of the umbilical cord (the cord does not attach to the placenta correctly and instead attaches to membranes outside the placenta), a bilobed placenta (when the placenta is split into two halves) or a succenturiate-lobed placenta (with a second or third placental lobe much smaller than the largest lobe).
Pregnancies diagnosed as vasa previa must be carefully managed to avoid severe blood loss and death of the infant.
What Is the Incidence Rate of the Anomaly?
Vasa previa is rarely reported and occurs in 1 in 2,500 births, with a fetal mortality rate estimated to be as high as 50% if not diagnosed prenatally. There is no known cause; it is an anomaly of placental attachment that can occur in any pregnancy.
Are There Risk Factors or Warning Signs?
Vasa previa might be present if any of the following conditions exist: a low-lying placenta, bilobed or succenturiate-lobed placentas, or velamentous insertion of the umbilical cord. Pregnancies resulting from in vitro fertilization or multiple pregnancies are risk factors for the anomaly.
Vasa previa can be asymptomatic but can also present with sudden onset of abnormally heavy or small amounts of painless vaginal bleeding in the second or third trimester of pregnancy. The source of the blood should always be investigated to determine whether the blood is maternal or fetal if the baby is not in distress.
The anomaly is not related to diabetes, obesity or high blood pressure.
How Is Vasa Previa Diagnosed?
Vasa previa can be detected during pregnancy with the use of transvaginal sonography in combination with color Doppler. The diagnosis often is made during the anatomy scan at 18 to 22 weeks of gestation. Routine obstetrical ultrasound protocols should include visualizing the placental cord connection for velamentous cord insertion, preferably with color Doppler. Any pregnancies suspected of velamentous cord insertion, placenta previa or low-lying placenta should be checked for vasa previa with transvaginal color Doppler ultrasound. Multi-gestational pregnancies and multi-lobed placentas also need to be closely monitored for vasa previa.
If there is any suspicion of vasa previa, it should be confirmed as the pregnancy progresses. After an early diagnosis and confirmation at around 28 weeks, the pregnancy should be closely monitored with regular ultrasound studies. As the placenta and uterus grow during pregnancy, the growth may move the vessels away from the cervix.
In General, How Is Vasa Previa Treated?
When diagnosed prenatally, treatment plans could include the following:
- Use of tocolytics to stop all uterine activity
- Total pelvic rest, including no sexual intercourse or vaginal exams other than transvaginal ultrasound, which has been proven to be safe
- Hospitalization in the third trimester, usually at about 30 to 32 weeks
- Regular ultrasounds to monitor progression of vasa previa
- Steroid treatment to develop fetal lung maturity
- Most importantly, elective cesarean delivery early enough to avoid an emergency but late enough to avoid complications of prematurity
Based on current research, 34 to 36 weeks may be the optimal time for delivery of vasa previa infants. When the anomaly is not diagnosed prenatally, aggressive resuscitation, complete with blood transfusion for the infant, may be necessary.
Every case of vasa previa is different, and any management plan should be developed in partnership between the mother and her doctors based on her own individual circumstances.
What Is the Prognosis?
Vasa previa is a serious condition. If the mother ruptures and bleeds at home, the baby will die in 95% or more of cases. If the mother’s membranes rupture while she is hospitalized on bed rest, the chance of fetal death remains about 50%.
When properly diagnosed and treated prenatally, the chance of the baby’s survival is very good. The fetal mortality rate is very low when an elective cesarean section is performed after fetal lung maturity is adequate.
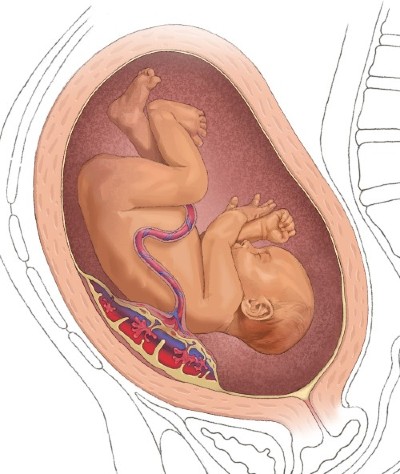
Normal Placenta with Normal Cord Insertion
In normal pregnancies, the umbilical cord is inserted in the center of the placenta, where it is protected.
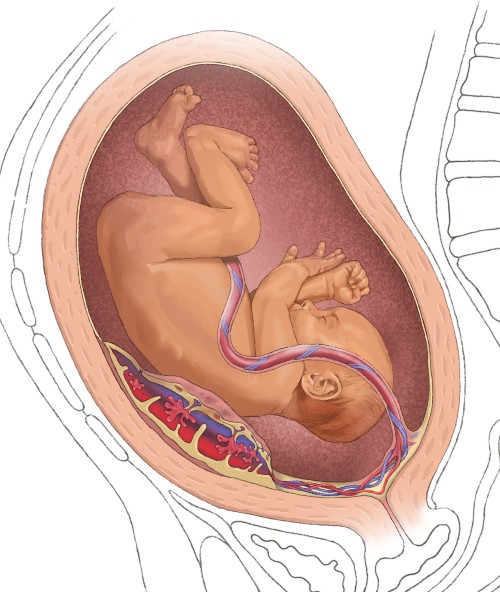
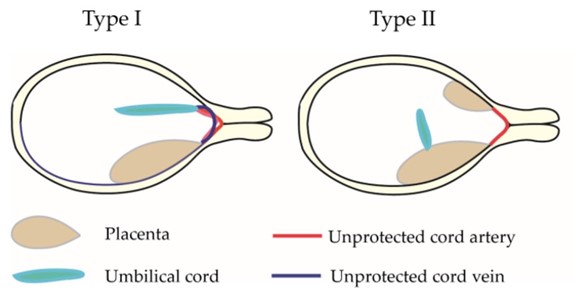
Type 1 Vasa Previa
In some pregnancies it attaches instead to the edge of the placenta, where it is at risk of breaking. If the attachment of the placenta to the wall is directly above the cervix, Type 1 vasa previa is diagnosed.
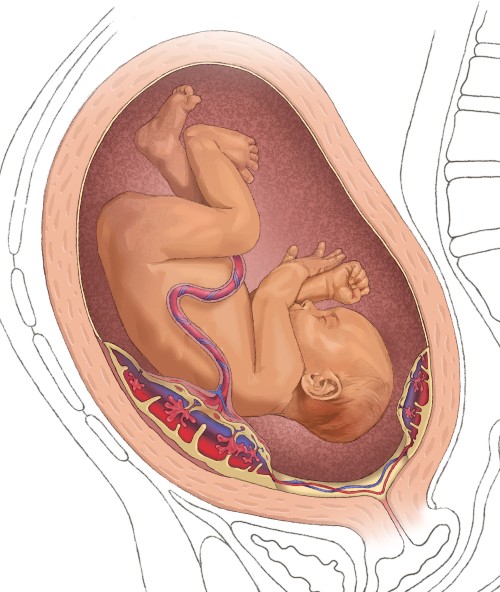
Type 2 Vasa Previa
In Type 2 vasa previa the placenta has two lobes. The large lobe has an umbilical cord connection and the smaller lobe, called a succinturate lobe, is attached to the main lobe through smaller vessels that travel over the cervical canal, with the umbilical cord connecting to the main lobe and connecting to the succinturate lobe. If the exposed blood vessels traveling between the lobes lie close to the cervix, they can burst and bleed when labor begins.
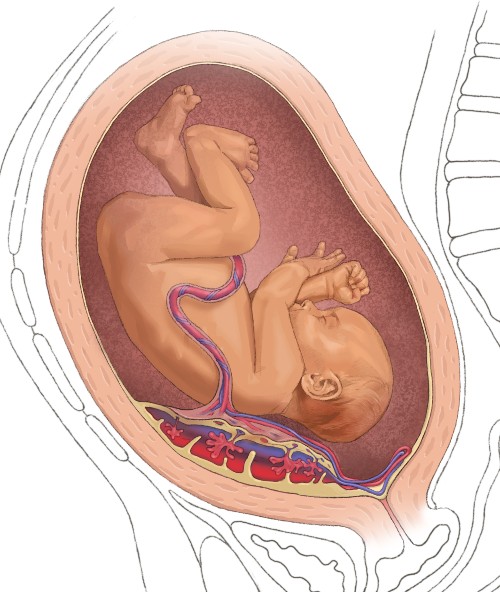
Type 3 Vasa Previa
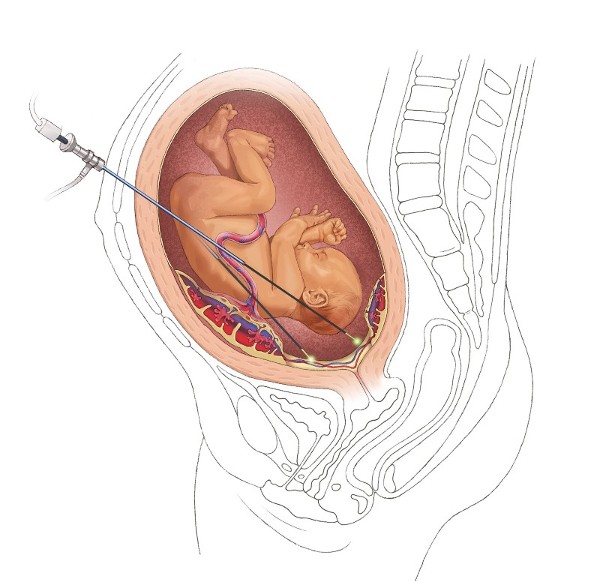
Fetoscopic Laser Ablation for Type 2 and Type 3 Vasa Previa
Maternal-fetal medicine specialists at McGovern Medical School at UTHealth Houston and Children’s Memorial Hermann Hospital successfully perform fetoscopic laser surgery to remove the blood vessel in pregnancies with Type 2 and Type 3 vasa previa. In a very select group of patients, fetoscopic laser ablation (FLA) is an option to continue the pregnancy to full term, avoid an unpredictable rupture of blood vessels and eliminate the need for a prolonged hospital stay. The procedure is done electively at 29 to 32 weeks, most often at 31 or 32 weeks.
Following the FLA procedure, mothers undergo continuous fetal monitoring for two hours and postoperative transvaginal ultrasound to confirm cessation of flow in the vasa previa vessel. Typically, they are discharged home on postoperative day 1. They are followed up with transvaginal ultrasound one week later. Afterwards, mothers may return to normal activity, with the option of being followed in an outpatient setting.
After the procedure, mothers can anticipate a vaginal delivery if there are no obstetrical contraindications. Some babies avoid a stay in the hospital’s Level IV Neonatal Intensive Care Unit.
Vasa Previa Resources for Clinicians
Papanna R, Agarwal N, Bergh EP, Brock C, Espinoza J, Johnson A. Fetoscopic laser ablation in pregnancies with Type-II vasa previa. Ultrasound Obstet Gynecol. 2023;61:773-781. PMID: 36609872. doi: 10.1002/uog.26153. Online ahead of print.
Contact Us
When you contact The Fetal Center, you will be in touch with a dedicated coordinator who will walk you through the process step-by-step and help you to understand every aspect of your care.
The Fetal Center at Children's Memorial Hermann Hospital
UT Professional Building
6410 Fannin, Suite 210
Houston, Texas 77030
Phone: (832) 325-7288
Toll free: (888) 818-4818
Fax: (713) 383-1464
Email: thefetalcenter@memorialhermann.org
To contact The Fetal Center at Children's Memorial Hermann Hospital, please fill out the form below.
Located within the Texas Medical Center, The Fetal Center is affiliated with McGovern Medical School at UTHealth Houston, UT Physicians and Children’s Memorial Hermann Hospital.